Learning More About Sleep Apnea In Women
Dr. Katherine Sharkey is a sleep medicine physician from Brown University and member of the Society for Women’s Health Research Sleep Network. She discusses sleep apnea recognition and treatment with a patient and a sleep technician. They discuss the challenges that women with sleep apnea often face, since the stereotypical patient is male (but that’s changing!). They also talk about how difficult adjusting to CPAP can be. Getting treated for CPAP can require patience to find the right solution that works.
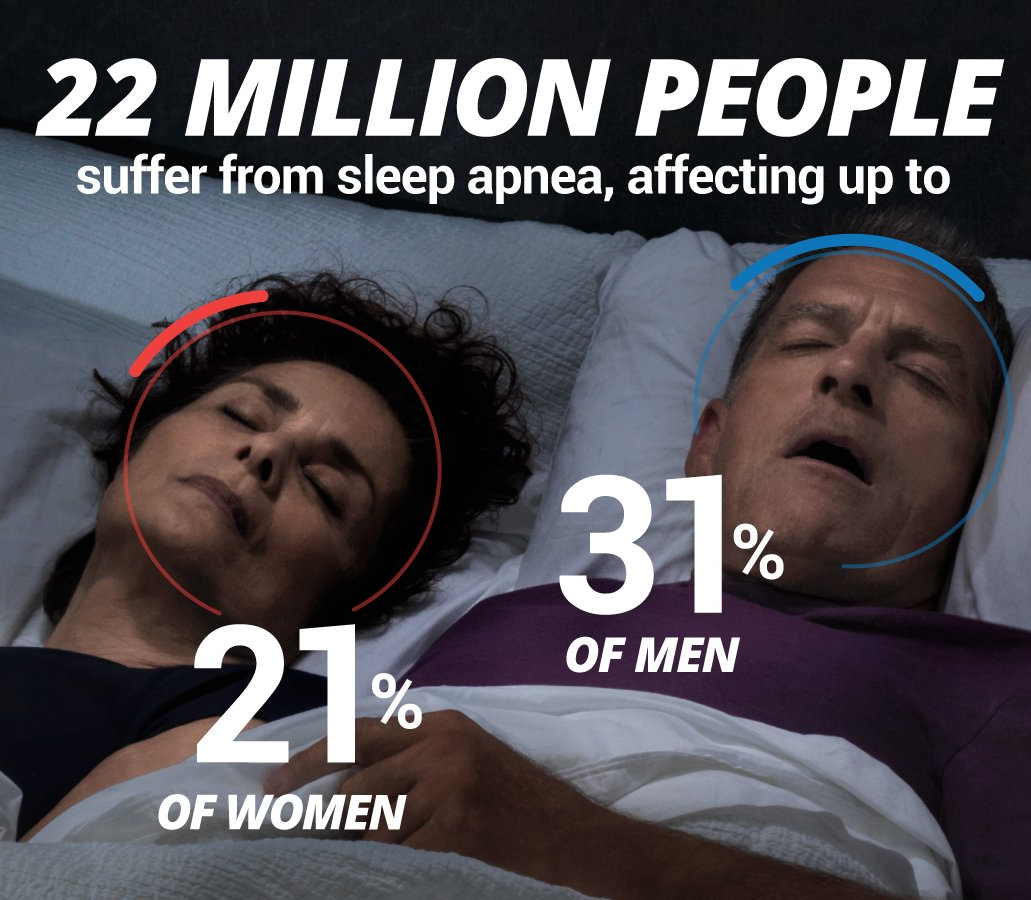
Sleep scientist and clinician Dr. Katherine M. Sharkey, who specializes in women’s health research, understands this well. “The poster person in someone’s head is a 60-year-old obese man. They’re not thinking of a young, marathon-running mom as someone having sleep apnea,” said Sharkey. Nor, necessarily, are primary-care professionals, who may hear from their patients accounts less disturbing than Foisy’s perilous driving and draw different conclusions.
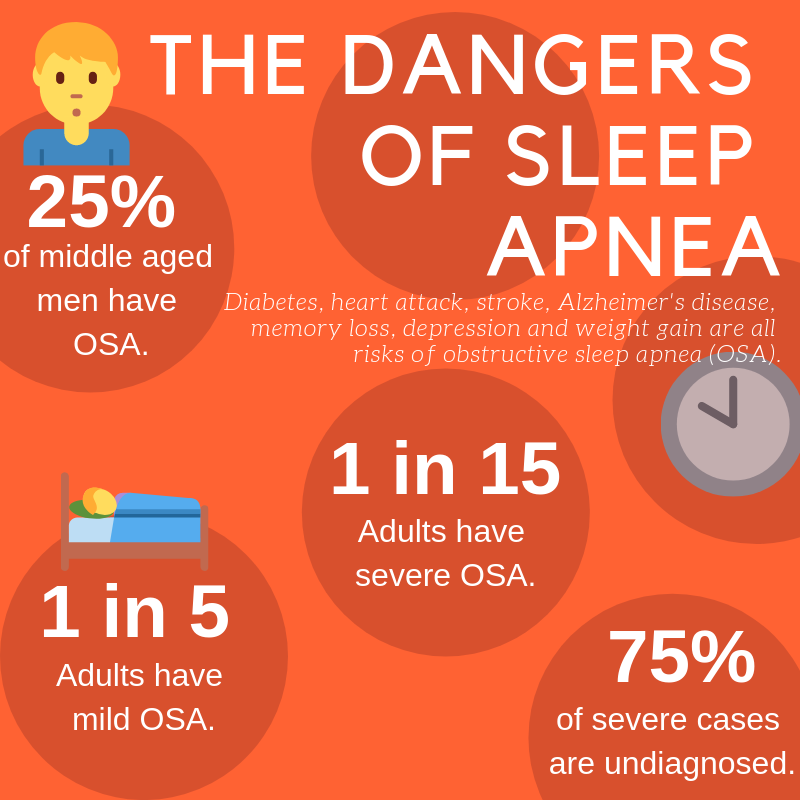
“In the past decade, rapid advances have been made in our understanding of the science of sleep and circadian rhythms and their essential role in health, well-being, safety, and productivity,” writes the Society for Women’s Health Research , headquartered in Washington. “The game changer is the mounting evidence that sleep and circadian rhythms regulate nearly all biological and behavioral processes, from molecules, single cells and [hormone] systems to whole body physiology and functions.” In other words, poor or inadequate sleep can negatively affect the whole being.
Obstructive sleep apnea, which Foisy experienced, happens when a person’s upper airway becomes blocked, stopping or reducing the flow of air. Causes can include a person’s unique anatomy, or medical conditions such as obesity, endocrine disorders and some genetic syndromes. (“Central sleep apnea” occurs when breathing signals from the brain are not sent.) Women lag men in recognizing and reporting for a multitude of reasons, according to Sharkey. For example, she says, “There’s the bias of, ‘Do I want people to know I snore? It’s not ladylike. It’s embarrassing.’”
Foisy overcame such inhibitions when she first sought medical attention in 2010, when she was a single mother with a 3-year-old. The condition was confirmed after a night in a Massachusetts sleep lab, during which her sleep patterns, brain waves, blood-oxygen levels and other vital signs were monitored. She began sleeping with a continuous positive air pressure (CPAP) machine, which keeps the airway open with a continuous flow of air delivered by tube to a face mask. But that early-era device was loud, uncomfortable and cumbersome, and eventually Foisy stopped using it. “Very primitive in terms of technology,” she said. “The mask was a challenge to fit right and cleaning was a pain.” Years later, she met Sharkey in a social setting, and they became friends. The doctor persuaded her to resume treatment — with one of today’s smaller, quieter and smaller CPAP devices that are easier to transport and clean.
Sharkey practices at the Brown Medicine Sleep Center in West Warwick, which features two sleep labs. The word “lab” is something of a misnomer: while the sleeping body is indeed monitored, the space resembles a comfortable hotel room, with bed, television, wall art, night table, chairs and soft lighting. And it’s quiet.
Chris Ruzzo, registered polysomnographic technologist, is master of this realm. She has been monitoring people with sleep issues for almost 35 years, and during that long career has accumulated great wisdom along with her technical expertise.
“You brain is like a computer: it needs to defrag itself” during restful sleep, Ruzzo says. “With fragmented sleep, your body wants to wake you up. But your brain’s trying to say, ‘Hey, I need to do what I need to do.’ But your body is saying, “Hey, I need to breathe.” There are no facile fixes. As Ruzzo put it, “You can’t take a pill and call it a day.”
And while other treatments are sometimes indicated, a CPAP device is typically preferred. Ruzzo recalled the days when health professionals “treated people who were on ventilators because they were so ill” and spoke of the evolution of a CPAP machine from Goldbergian contraptions to today’s miniature versions. “They have travel CPAPs that are the size of your cellphone,” she said. Foisy has been a beneficiary, as evidenced during a recent trip that she, her son, and her partner and two of his young children recently took to theme parks in Florida.
“We were doing 10 to 15,000 steps a day, three kids running around, going through the parks,” she said. “I wore it every single night — and every single morning, I woke up between 5 and 6 o’clock on my own saying, ’I’m done sleeping, I’m rested, I’m ready to get up and face the day.” And not just vacation days, Foisy told The Journal. “Boy, do I notice a difference when I don’t use it for a night or two,” she said. “I wake up in a haze, tired and begrudgingly starting my day — in contrast to this morning, when I woke up fully rested, ready to tackle the day after a full night of healthy breathing and sleep.”
Is it apnea? What to do?
Daytime clues
- Feeling depressed, anxious, irritable or impatient
- Feeling tired, drained or lacking energy
- Feeling sleepy or falling asleep at the wrong time or place
- Forgetfulness, foggy or fuzzy thinking, trouble with focus and concentration
- Accident proneness
Nighttime clues
- Frequent or loud snoring, gasping, or snorting sounds
- Difficulty falling asleep or frequent awakenings
- Restless sleep or changes in dreaming
- Frequent bathroom visits at night
- Nighttime heartburn
What to do
“Sleep apnea is treatable. It is important to start a conversation with your health-care provider to discuss whether you are at risk for sleep apnea or another sleep disorder.”