College & Pro Sports Are Taking Sleep Seriously
Lebron James has reported to ESPN that he sleeps an average of 12 hours each night. Usain Bolt, Venus Williams, and Maria Sharapova average ten. By comparison, the average American sleeps seven hours. Reflecting on that simple fact stresses the importance of sleep for the body’s overall performance — the body recovers during sleep, and professional athletes strain their bodies to the limit every day.
Athletes and the Importance of Sleep Education
Clearly, sleep is necessary, not optional, for sports players to perform in the mind-boggling manner we see on TV. While coaches have recognized for some time that sleep is important for players’ performances, there has recently been an increased focus on sleep education that is changing the way professional sports view the issue. The NCAA Board of Governors named adequate sleep, nutrition and performance as a top priority for college athletes this year.
In May, the new Interassociation Task Force on Sleep and Wellness , which is made up of coaches and student athletes, as well as leaders in sleep research, sports medicine, sports psychology, academic advising and mental health, convened for the first time at the NCAA’s headquarters in Indianapolis. The Association’s mission is to change the current culture around sleep, so college athletes and coaches no longer leave quality sleep out of nutrition and wellness routines. Among other goals, the task force aims to create sleep guidelines that can be distributed to college athletic departments nationwide.
Why Professional Athletes Need Sleep
And the issue has recently gained awareness in professional sports, too. Dr. Charles Czeisler, a recognized expert for professional sports teams and the director of the Division of Sleep Medicine at Harvard, has attempted to bring to light the importance of sleep for athletes in recent years. He has addressed that players who don’t get a full night’s sleep after practice will never be able to form long-term memories.
Sleep is what turns new memories into long-term ones as the brain rebuilds itself after a long day. Without that process each night following a day’s practice, athletes will never properly file away the facts from that day or integrate lessons into existing knowledge.
Furthermore, prolonged sleep deprivation has been shown to have devastating effects on the body and overall health. While everyone is susceptible to the consequences of sleep deprivation, athletes are particularly at risk due to the amount of stress they put on their bodies during their careers.
How NFL Players Are Fighting Sleep Apnea
For the Pro Player Health Alliance (PPHA), tackling sleep apnea in pro athletes is their mission. Founded in 2012, the alliance is made up of David Gergen, CDT and President of the PPHC and a practicing dental lab expert for over 25 years, as well as former NFL players, including Roy Green, Derek Kennard, and Mike Haynes. Each player in the alliance has been diagnosed with sleep apnea, and have been successfully treated using oral appliance therapy. Most notably, former NFL wide receiver Roy Green insists that his sleep apnea condition contributed in large part to the multiple life-threatening episodes he suffered prior to his diagnosis.
In one interview with Gergen, Green said, “I’ve had two strokes and two heart attacks previously. There’s no question in my mind that… the fact that I wasn’t getting enough oxygen, I wasn’t sleeping, that I was tired all the time, that definitely played a part in it.”
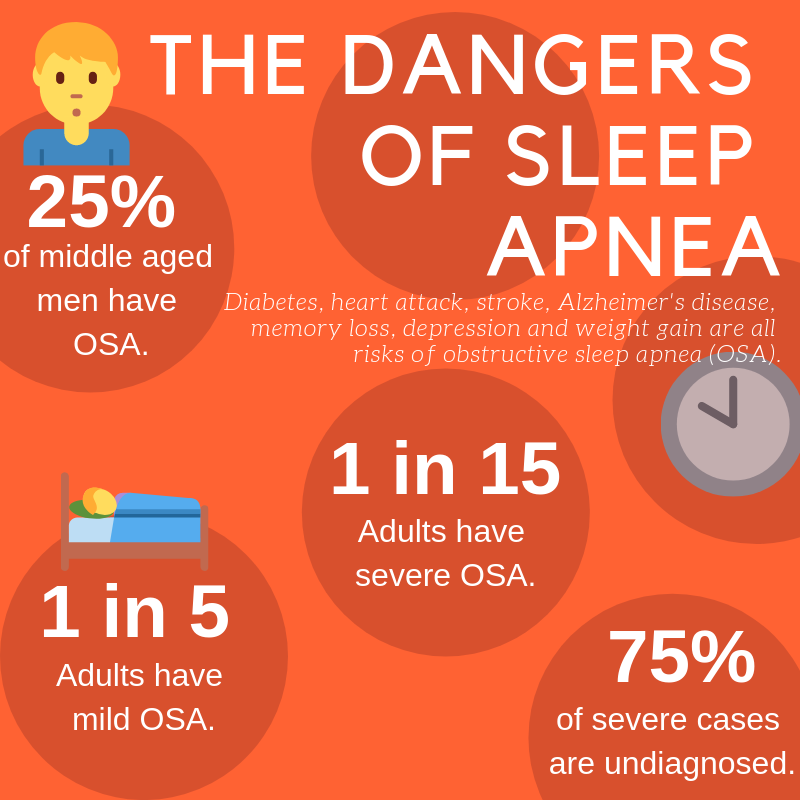
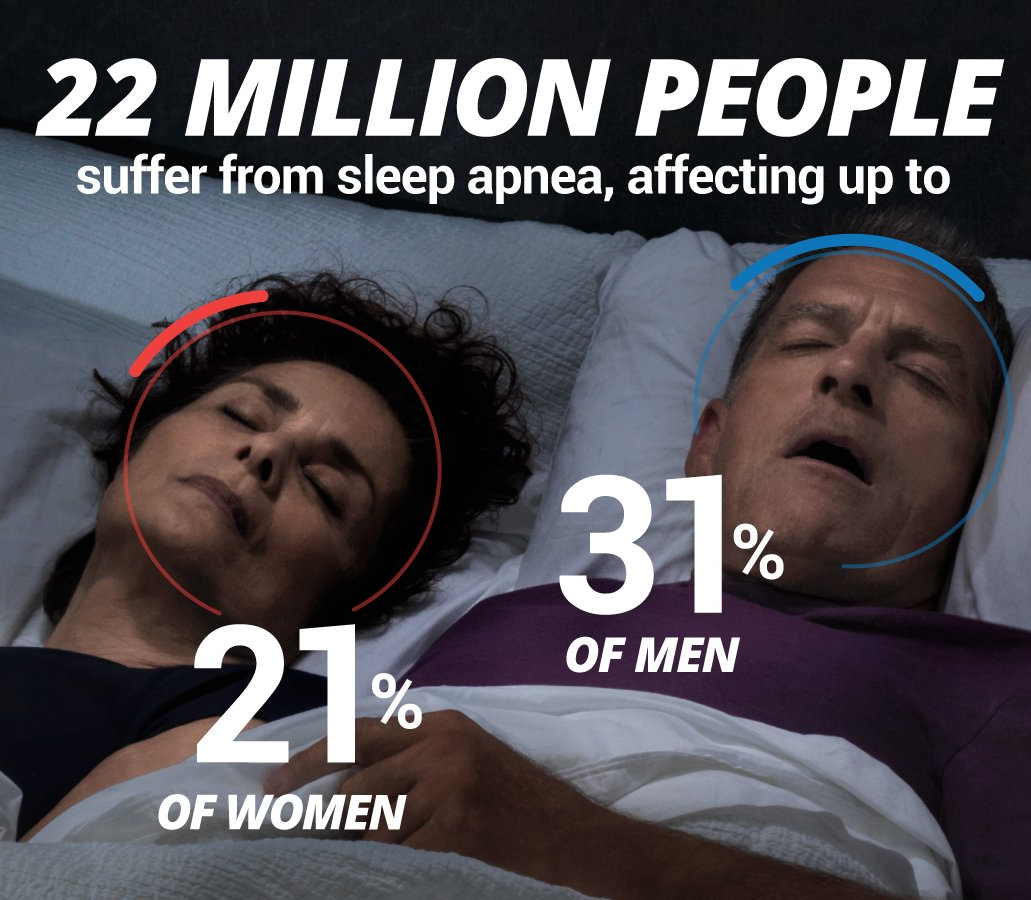
The PPHA is dedicated to increasing awareness of sleep apnea in professional football players so they can get treatment and have a better quality of life. The PPHC has visited schools and held meet-the-players and other events for fans, all to promote the alarming prevalence of sleep apnea in football players. One study found that 60 percent of NFL linemen and 46 percent of players in other positions suffer from the disorder.
The American Sleep and Breathing Academy
David Gergen is also CEO of the American Sleep and Breathing Academy (ASBA), which was founded to improve patient care through “education for sleep professionals, sleep centers, patients and the community at large.” The nonprofit’s goal is to strengthen the sleep profession via a multidisciplinary approach, focusing largely on the awareness of oral devices as treatment.
In an interview with the American Sleep and Breathing Academy, Mike Haynes said, “I think that if players knew the importance of sleep, they would want to improve it. I think that they just don’t know. They think five or six hours of sleep is fine, and if they are on time, they are ok.”
He goes on to say that he thinks oral appliance therapy is the best way to treat sleep apnea in players, as they’re used to mouthguards.
Gergen, along with Sleep Dallas’ Dr. Kent Smith, who is President of ASBA, and members of the PPHA have recently visited Washington, D.C. to present to a Caucus Committee of the U.S Senate about the effectiveness of oral appliance therapy as a treatment option for sleep apnea. The organization continues to lobby in D.C. for the issue.
Gergen says, “The goal is to make oral appliances the true benchmark for mild to moderate sleep apnea,” according to a press release by the American Sleep and Breathing Academy.
What This Means For the Rest of Us
The recent shift in awareness about sleep deprivation and how it affects athletes’ performances is a positive one for sleep education across the board. Whether you’re training for the playoffs or sitting at a desk, poor sleep wreaks havoc on the body. It impedes your brain’s reaction time, drains focus and memory, and affects decision making skills. Quality sleep is absolutely critical for overall health and wellness, and will help ensure your life is as full and productive as possible. The post College & Pro Sports Are Taking Sleep Seriously appeared first on Sleep Dallas Blog.